A new study suggests the cost of diabetes burden in sub-Saharan Africa could more than double, costing the region up to $59.3 million a year by 2030, if type 2 diabetes cases continues to grow.
The study proposes diabetes—and its complications—could potentially reverse health gains seen in the region in recent years.
It would overwhelm health systems and crippling personal finances of patients as they continue to pay for their own healthcare.
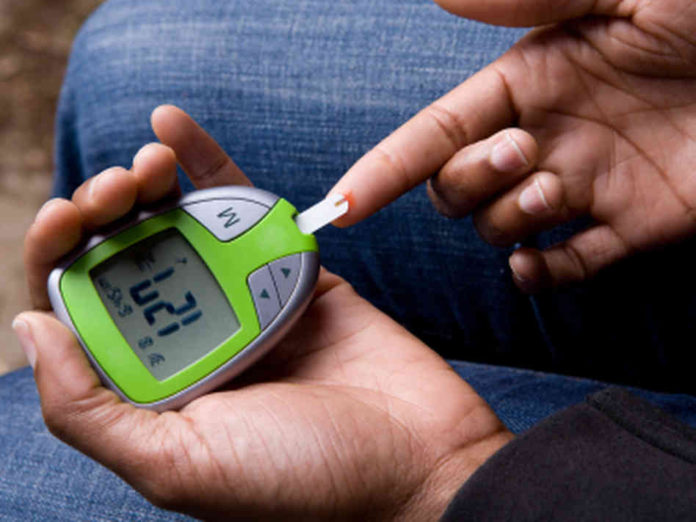
Only one in two people with diabetes know they have the condition, and just one in 10 of them receive drugs they need.
The report of the study, Lancet Diabetes & Endocrinology Commission on diabetes in sub-Saharan Africa launched on Thursday in London.
In 2015, diabetes cost the region’s economy $19.5 billion—equivalent to 1.2% of gross domestic product.
Countries in the region spend up to 5.5% of their GDP on health. More than half the spending, around $10.8 billion, was on access to diabetes treatment—and half the total cost was paid by patients.
The other economic costs came from loss in productivity: early deaths shaved $7.9 billion off the region’s ecnomy; people leaving the workforce early cost $500 million; sick leaves took away $200m and lower productivity due to poor health cost $70m.
Rifat Atun, lead author on the report and a professor at Harvard University, USA, said, “These estimates show the vast economic burden that diabetes places on sub-Saharan Africa, and should motivate policy makers to increase resources and efforts to overcome this looming health challenge.”
“Our figures illustrate the economic cost of inaction,” she added.
“However, the wider cost of inaction is the risk of losing ground on some of the region’s biggest health achievements of the past few decades, as diabetes cases further increase and costs spiral. In its current state, sub-Saharan Africa is not at all prepared for the increasing burden of diabetes caused by rapid, ongoing societal transitions.”
To measure the future impact of increased diabetes rates across all sub-Saharan African countries, the researchers modelled three scenarios to show optimistic and pessimistic projections. Their estimates suggest that, in an optimistic scenario, where diabetes death rates and prevalence remain the same for each country, the annual cost of diabetes would increase to $35.3 billion (1.1% GDP) in 2030.
However, if these rates increased in line with the projected rise in each countries’ income levels, economic costs would be $47.3 billion (1.4% GDP), and if rates doubled, the costs could total $59.3 billion (1.8% GDP).
Wealthier areas of sub-Saharan Africa seeing more societal changes had the highest rates of diabetes in 2015, with almost two-thirds of the region’s diabetes costs coming from southern Africa (62%, $12.1 billion), in particular, wealthier South Africa.
Less than a tenth of the costs (9%, $1.7 billion) originated from poorer countries in western Africa.
In the projections for 2030, southern Africa is likely to see the greatest increases in annual costs, increasing to between $17.2 and $29.2 billion.
However, the authors also predicted substantial growth in costs in eastern African countries (such as Ethiopia, Kenya and Tanzania), increasing from $3.8 billion in 2015 to up to $16.2 billion in 2030.
The Commission’s analyses demonstrate a clear need for improvements at all levels of diabetes care. However, after decades of treating acute infectious diseases, health systems in sub-Saharan African countries are ill-prepared to handle the chronic disease.
The authors of the Commission report conclude that gaps in care include a lack of equipment for diagnosing and monitoring diabetes, lack of treatments, and lack of knowledge about the disease among available healthcare providers.
These gaps contribute to the fact that half of patients go undiagnosed, while only one in 10 (11%) receive the drugs they need.
Many patients face delayed diagnosis and treatment, meaning the disease progresses and causes further ill health and risk of complications, for example myocardial infarction, blindness, and stroke, which are difficult and expensive to treat.